It started with a weird breakout on his face.
So Tommy Dennis, who was 22 years old at the time, had the bumps checked out by an Omaha dermatologist. The doctor told him that the breakout looked like the symptoms of a potential HIV infection. “Then he ordered a blood test. I came back a week later and found out that my test came back positive.”
Dennis, who is now 35, was devastated.
In the United States, more than 30,600 people ages 13 and older were diagnosed with human immunodeficiency virus, the virus that causes AIDS, in 2020. More than 1.2 million people are living with it.
In Nebraska, the number of new HIV diagnoses hit 107 in 2021, up from a yearly average of 81, state health officials said, noting that a drop in HIV testing during the COVID-19 pandemic is at least partly to blame for the increase. The spike occurred primarily among white men, mainly in the state’s rural areas.
However, since the beginning of the HIV/AIDS epidemic, Black Americans have been disproportionately affected, and that disparity has deepened over time, as the KFF health policy group notes.
Although they represent only 12% of the population, Black people account for a much larger share of HIV diagnoses (42%), people living with HIV (40%) and HIV-related deaths (43%) than any other racial or ethnic group in the U.S., according to 2020 figures reported by the Centers for Disease Control and Prevention.
NEBRASKA HIV UPDATE
Nebraska health experts will present a daylong “Nebraska HIV Prevention and Care Update” on Thursday, May 18, at the University of Nebraska at Omaha’s Barbara Weitz Community Engagement Center from 7:45 a.m. until 5 p.m. Topics to be covered include barriers to HIV prevention, treatment disparities, aging with HIV and what’s new in HIV care. Although the conference is at capacity, people can attend virtually by going to bit.ly/UNMC-HIV.
The disparity persists in Nebraska, where Black people, who make up 5% of the population, accounted for 21% of new HIV diagnoses in 2021. That reality, according to advocates and health care providers, can make seeking care onerous for patients and complicate providers’ ability to deliver treatment that is much more effective and causes fewer side effects than earlier treatments.
Dennis, who is Black, went to work at the Nebraska AIDS Project in 2017. “I was charged with basically developing a program to do outreach toward Black same-gender-loving men and really try to promote (HIV) testing efforts in the community, which, you know, in large part has been successful … But I think there is such a level of medical mistrust when it comes to testing — in minority communities especially.”
Lack of access to health care also is an issue for minority populations, said Dr. Nada Fadul, a professor in the University of Nebraska Medical Center’s Division of Infectious Diseases. Fadul is the medical director of the UNMC Specialty Care Center in Omaha, where 1,200 HIV patients — a little more than half of all HIV patients in Nebraska — are treated.

For some people, Fadul said, issues such as a lack of transportation, food insecurity and/or difficulty finding housing play a role in their not getting treatment. Distrust in the health care system also factors in.
Dennis still bristles at the way the first doctor told him he was HIV-positive.
“He didn’t even bother closing the door,” he recalled. “He stood in the doorway and basically said, ‘Yep, your test results came back positive. I’ll send the nurse in with a referral, and we’re going to get you on your way.'”
Fadul said some medical providers still have unconscious bias against racial minorities and the LGBTQ+ community.
“Patients feel that,” she said. “If I walk into a clinic and the doctor is looking at me (disapprovingly) or saying words that imply that I’m less of a person, I’m not going to come back. I’m not going to feel comfortable in this clinic.”
Whether providers look like the people they serve also matters, Fadul said.
“If 30% of my patients are Black,” Fadul said, “then I need to have representation of that population in my workforce. So when patients walk into the clinic, they can see that, ‘Oh, there are people who look like me, talk like me, dress like me, so I can feel comfortable in this environment, I can feel safe.'”
If they can overcome the initial barriers, people with HIV can begin a fairly simple treatment regimen, albeit one they will have to continue indefinitely.
HIV medications today have fewer side effects than they used to, and they’re easier to take.
In March 1987, AZT became the first drug to get FDA approval for the treatment of AIDS.
“It was something,” Dr. Susan Swindells said, “but it was really a pretty awful drug. We gave people big doses of it, five times a day. I used to have to tell people, ‘Set your alarm for 2 o’clock in the morning, wake yourself up and take this medicine.’ … And it generally made people feel terrible. On average, they lived about a year longer than they would without it.”

Swindells, a professor of medicine and longtime HIV researcher at UNMC, said treatment didn’t improve until the mid-1990s, with the introduction of new medicines called protease inhibitors. “That turned the corner,” she said. “That made people better, and they stopped dying.”
Cindy White remembers the harsh drugs. She said her friends with AIDS used to call AZT “rat poison.”
White, who is 62, figures she contracted HIV from a man she was dating in 1984 while living in Denver.
White had gotten really sick that summer, spiking a temperature of 104 degrees, but she recovered from that while the HIV quietly continued to build up in her, damaging her immune system.
After breaking up with the guy, she met her future husband in early 1985, and they moved back to Omaha, where White grew up. They divorced about four years later after having a son together.
Then her ex contacted her in 1990 after he had tried to sell plasma. A sample of his donation had been found to be HIV-positive.
“He called me everything,” White said. “You know, like, everything. ‘I’m gonna die. It’s your fault.'”
Then she phoned the man she was seeing to give him the news. “Well, you gotta go get tested,” he told her. “And I said, ‘Well, you gotta go get tested.'”
She and her boyfriend eventually both tested HIV-positive — her first, then him a few months later. Four months after the diagnosis, White was found to have no immune system and “officially” had AIDS, which kicks in when the number of infection-fighting “CD4” cells drops below a certain level.
“Then it’s kind of game on,” White said. “Because with such a low immune system, everything made you sick.”

Eventually, White said, “the virus beat my immune system down to a point that it reactivated an infection called cytomegalovirus and it took my eyesight.” She has been blind ever since.
After being on AZT, plugging into various drug trials — at one point taking about 100 pills a day — plus going through chemotherapy, White was down to 95 pounds and “wasn’t in good shape.”
Her doctor started her on a new drug that White said made her weight skyrocket, requiring her to wear size 3X clothes. But it worked on her HIV infection, and her viral load was undetectable about two years after she started taking it.
White stayed on that drug for about 20 years after her doctor adjusted the dosage. Her weight gradually returned to normal.
White’s boyfriend, who also had been on several HIV drug trials, died of a fungal infection in December 2001. Her ex-husband died in 2005.
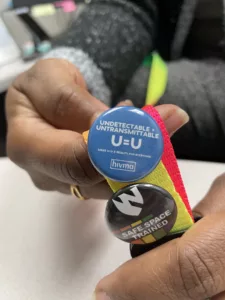
Today, people with HIV who stick with their treatment can get their viral levels down to basically zero and can’t transmit HIV, a concept dubbed “U Equals U” — undetectable equals untransmittable.
“If your viral load is undetectable, meaning that you’re taking medications, they’re wiping out the viral load in your blood,” Fadul said. “You’re not going to transmit HIV sexually to your sexual partners. And this is a proven fact, you know, thousands and thousands of patients have been studied — using condoms, not using condoms … There is no transmission.”
And people today also have access to PrEP medicines — Pre-Exposure Prophylaxis, which reduces the risk of getting HIV from sex by about 99%. Dennis, Fadul and Swindells all noted that PrEP can keep you from getting HIV, but it can’t stop you from getting chlamydia or gonorrhea or herpes.
“We understand condoms aren’t everybody’s thing,” Dennis said, “but we still encourage folks to use them. And if you’re not going to use them then you should be getting tested (for HIV) often.”
Testing is important — an estimated 13% of people in the U.S. with HIV don’t know they have it, so if they’re sexually active, they’re spreading it to their partners. The CDC recommends that everyone between the ages of 13 and 64 be tested at least once, and people who are in certain high-risk categories should be tested at least once a year. (And it’s not just gay or bisexual men — people who acquired HIV through heterosexual contact made up 22% of HIV diagnoses in the U.S. in 2020.)
For more information, contact the Nebraska AIDS Project at nap.org.
The Flatwater Free Press is Nebraska’s first independent, nonprofit newsroom focused on investigations and feature stories that matter.



1 Comment
Thank you for such a comprehensive, compassionate story about HIV. I began to volunteer with NAP in 1988 and have watched this disease change and mutate ever since. I watched many new friends perish and then many more thrive. Science Rules! Dr. Swindells and Dr. Howard Gendelman have done miracles for Nebraska and for the global HIV+ population.
Thank you for the lovely story about my dear friend, Cindy White, and her beloved Scarlet.